Top Stories
Pelvic organ prolapse (POP) – Embarrassingly common? – Help is out there
By Preetkiron Bhal
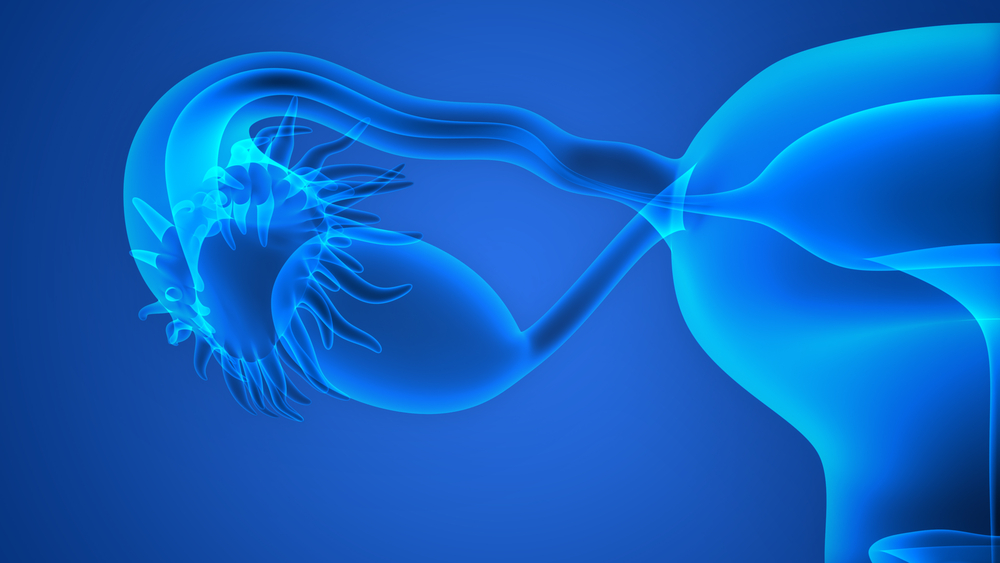
What is pelvic organ prolapse?Any organ in the female body like the bowel, bladder, and womb can drop out of place. These result in a condition called pelvic organ prolapse (POP). If these organs are no longer in their normal positions and if this condition is not taken care of, quickly enough, these organs can fall farther into the vagina. POP is a very common condition which affects up to 1 in 3 women especially if they have had children.
The various types of POP which include cystocoele (prolapse of the bladder), hysterocoele (prolapse of the uterus), rectocoele (prolapse of the rectum), enterocoele (prolapse of small intestine), and vault prolapse (prolapse of the top of the vagina in women who have had a hysterectomy). Often more than one type of prolapse may occur at the same time.
What are the causes of POP?
The weakening of the vaginal support system results in this condition. There are several causes linked to POP. These include:
- A lack of oestrogen (female hormone) following the menopause weakens the pelvic support structure that relies on this hormone for their strength.
- Pregnancy places a high degree of stress on the various tissues, ligaments and muscles of the pelvic floor which can also tear during childbirth thus resulting in this condition.
- Hysterectomy which is surgery that involves the removal of the uterus that is a very important part of the support network complex in the pelvis can cause a drooping of the upper part of the vagina leading to a vault prolapse.
- Other causes include ageing, chronic constipation, obesity and certain connective tissue disorders.
This will depend on the kind of prolapse that you are suffering from however; the most common symptom is the experience a dragging sensation or sensation of something that has come down in the vagina. Other symptoms may include pelvic discomfort or a lack of sensation during intercourse, difficulty having a bowel movement or bladder weakness leading to incontinence.
How is this condition diagnosed?
If you believe you are experiencing symptoms associated with POP, you should seek a consultation with a specialist in pelvic floor problems. During the initial evaluation, the specialist will take a detailed medical history, looking for factors that may have contributed to this condition and perform a thorough pelvic examination.
Your doctor is likely to measure the position of your uterus to determine how severely it has dropped or "prolapsed". In addition, part of the exam may sometime be performed while you are standing to gauge the severity of the condition. The doctor may ask you to bear down like you were having bowel movement or cough. These actions make the pelvic injury more obvious.
Diagnostic tests, such as urodynamic studies to evaluate bladder function or special imaging studies to visualise the bladder or rectum may subsequently be arranged.
What can be done for POP?
Not all women with POP have symptoms that require treatment. The treatment that is best for you will depend on many things – your symptoms and their effect on your life, your age and your plans for pregnancy, and your expectations for treatment.
Intensive and regular pelvic floor exercises help by both strengthening and relaxing the pelvic floor muscles so they become firm and supportive, but not overactive. Many women will have a major improvement in or recovery from symptoms of prolapse by learning effective pelvic floor exercises, thus avoiding or delaying the need for surgery. It is important to learn to do the exercises in the right way, and to check from time to time that you are still doing them correctly. Hence it is recommended that women see a specialist pelvic floor physiotherapist to take them through these exercises. Women who require surgery usually have a much better result if they work with an experienced physiotherapist before and after their procedure.
In addition to exercises women may find medication such as oestrogen replacement or basic health and lifestyle changes such as dietary change or treating constipation and managing to lose weight may bring relief to their symptoms.
A vaginal pessary to support the prolapse is a good short or long-term solution. Short-term pessary use is appropriate for women to make them more comfortable if a planned surgery needs to be delayed. Some women with slight prolapse are only symptomatic at certain times, such as when they are playing golf or tennis, and find a pessary useful on an as-needed basis. There are multiple types of pessaries, and finding the right pessary in the right size is the key to success. Some women have had a negative pessary experience and feel as a result that they are not a good candidate, when in fact the pessary was the wrong type or did not fit properly.
These conservative treatment options are usually offered to most patients before considering surgery. However if these fail and the symptoms are compromising the quality of life significantly then surgery to repair the prolapse is an option.
Pelvic reconstructive surgerycan be performed through the vagina or abdominally (via a traditional incision or through laparoscopy/ ‘key-hole surgery’). During the procedure, the surgeon will reposition the prolapsed organ(s) and secure the surrounding tissues and ligaments. The vaginal defect(s) which cause the bulge in vagina will also be repaired. Usually a repair of the perineum to support the opening of the vagina may be performed. Prior to undergoing surgery, patients should undergo a thorough evaluation to ensure a proper diagnosis. For example, some women may have stress urinary incontinence (leaking with coughing or sneezing) and may require a sling procedure performed at the same time to correct urinary incontinence, however in some circumstances this is best done as a two stage procedure which will be discussed with your doctor. Surgery for prolapse has three key issues which are:
- failure of treatment of recurrence of symptoms
- the chance of developing new troublesome symptoms such as worsening incontinence, pain due to scarring or pain with sex and change in bowel habit
- complications of surgery including infection, bleeding, rarely injury to the surrounding organs
Therefore surgery to improve prolapse symptoms needs to considered ideally when all other options have failed and when the patient’s quality of life is severely affected enough to merit accepting the above key issues.
Many women are embarrassed about seeking treatment for pelvic organ prolapse. Prolapse often causes women to feel embarrassed and needlessly self-conscious despite it being so common. The possible reason is that women rarely feel comfortable talking to their friends and family about such intimate matters. The good news is that women do not have to suffer in silence and live with the condition. Seek help early and women can be empowered to do something about pelvic organ prolapse, and they will have choices to suit their individual needs.
Please visit http://www.iuga.org/?patientinfo for more valuable patient information leaflets on prolapse and its treatment options.
Preetkiron Bhal has been a Consultant Gynaecologist in Cardiff since 2003 with an interest in urinary incontinence, pelvic organ prolapse, general gynaecology and infertility. Mr Bhal is an expert in advanced vaginal and laparoscopic surgery. He offers a comprehensive service for managing urogynaecological problems including vaginal mesh related problems. Mr Bhal leads a multidisciplinary team in Cardiff striving to deliver the best available care for patients with bladder and pelvic floor conditions in South Wales. Mr. Bhal has continued with his passion for research and evidence based medicine and has presented work at numerous meetings both nationally and internationally.
Preetkiron can be contacted on +44 (0)333 800 8082 or by email at info@infinitihealthcare.com



Comments